Trying to figure out the best approach to move ahead with telemedicine app development for your business? Or need clarity on the right features, integrations, APIs, and compliance layers required to ensure scalability and ROI from day one. This section will help you understand the core fundamentals and strategic considerations necessary before hiring a telemedicine app development company or initiating your internal planning process.
Post COVID, remote care became a permanent part of healthcare delivery, pushing huge demand for telemedicine app development across startups, hospitals, clinics, and specialty practices. According to Grand View Research, the global telemedicine market is projected to reach USD 169.45 billion by 2030, demonstrating the rapid adoption of virtual care as the new standard in modern healthcare access.
Today, healthcare providers are investing in telemedicine app development to optimize consultations, improve patient experience, and scale revenue beyond physical boundaries. Some platforms support general care, while others require custom builds for specialized diagnostics and condition-focused workflows.
With AI triage, wearable data sync, voice interactions, and EHR interoperability becoming standard, telemedicine innovation is accelerating fast. Before diving into features or cost, it’s important to understand what this model means for the future of digital healthcare delivery.
What is a Telemedicine App?
A telemedicine app enables patients to connect with healthcare professionals remotely for consultations, diagnoses, and follow-ups. Telemedicine app development focuses on building secure, seamless platforms that support virtual care, remote monitoring, and real-time communication. It helps eliminate geographical barriers, improves patient engagement, and enhances care delivery across both urban and remote regions.
Example: Accuster Telemedicine Diagnostic App
Ment Tech helped Accuster build a mobile-first diagnostic platform that connects directly with biomedical devices, enabling faster testing, instant report generation, and seamless data sync across both field and clinical environments.
Custom vs. Ready-Made Telemedicine App Development. Which Option Is Right for You?
When developing a telehealth platform, one key decision is choosing between a custom-built solution or a ready-made telemedicine app.
1. Ready-Made Telemedicine Apps
These are quick-to-launch, affordable solutions ideal for clinics, small practices, or early-stage startups. They help you test the market faster but come with limited customization, restricted scalability, and fewer options for a unique user experience.
2. Custom Telemedicine App Development
Custom apps are built specifically around your healthcare workflows, compliance needs, and future growth roadmap. They require more time and investment initially but enable deep personalization, unlimited scalability, advanced tech integrations, and stronger brand differentiation.
Benefits of Telemedicine App Development
Telemedicine app development enables care delivery beyond physical boundaries, improving access, operations, and patient experience. It’s especially beneficial for Healthcare Startups building scalable, digital-first medical platforms with better long-term outcomes.
• Increased Accessibility
Telemedicine apps eliminate geographic constraints and make specialist care reachable for patients in remote or underserved regions, expanding access beyond physical hospital boundaries.
• Improved Patient Engagement
Easy digital booking, secured communication, reminders, and health record access keep patients consistently involved in their treatment journey, supporting adherence and better clinical outcomes.
• Cost Savings
By reducing unnecessary physical visits and automating admin workflows, providers lower overhead, save staff time, and optimize operational expenditure across the care delivery cycle.
• Enhanced Efficiency
Integrated scheduling, billing, triage, and documentation systems reduce manual processes, shorten turnaround time, and improve coordination between care teams inside healthcare environments.
• Better Health Outcomes
Virtual consultations and remote monitoring enable early interventions and continuous patient evaluation, ensuring timely care delivery and improved long-term recovery trajectories.
Recent Telemedicine Momentum Update
In 2025, India’s RMLIMS Lucknow launched a telemedicine pilot where patients can upload reports and consult doctors via video, reflecting rapid adoption even in government hospitals. Meanwhile, Hong Kong’s 2025 Policy Address announced major investment in telehealth infrastructure, AI-powered screening, and cross-border digital health records, signalling a strong global government-led acceleration of virtual care.
Top Use Cases of Telemedicine Apps
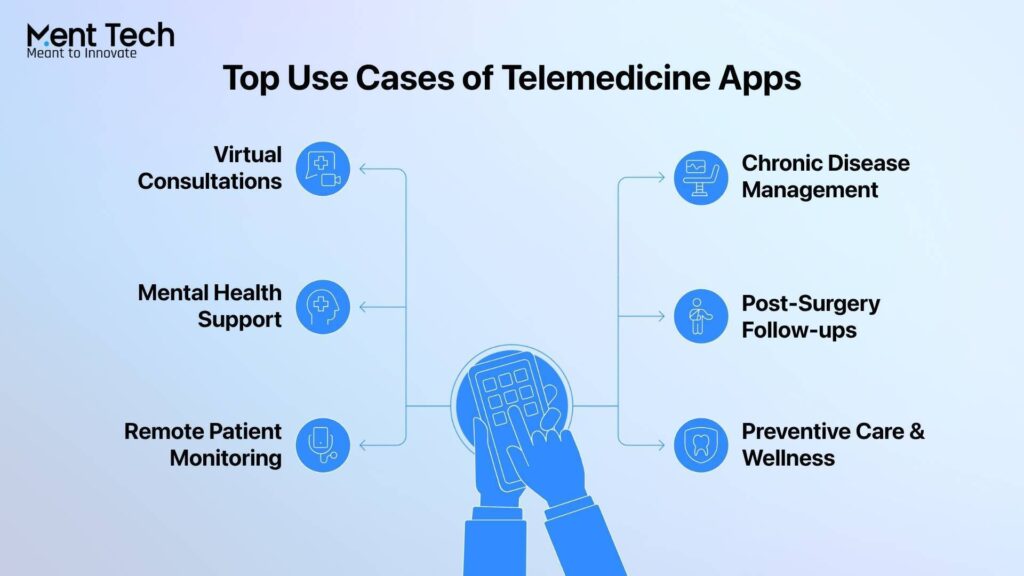
Telemedicine app development enables patients to instantly connect with doctors through secure video/voice calls, eliminating travel and wait time, similar to how a Personal Fitness Coach guides remotely. This is the most widely used telemedicine use case today.
1. Virtual Consultations
Telemedicine app development enables patients to instantly connect with doctors via secure video or voice calls, removing travel, long queues, and unnecessary wait times. This remains the most widely adopted use case across leading telemedicine app development companies.
• Real-time video/audio consultations
• Ideal for routine care & follow-ups
• Faster medical advice in minutes
2. Chronic Disease Management
Continuous remote monitoring helps doctors manage long-term conditions like diabetes, hypertension, and cardiac health without frequent hospital visits. Telemedicine apps ensure treatment stays aligned and proactive.
• Regular check-ins & vitals tracking
• Personalized treatment optimization
• Prevents complications through early action
3. Mental Health Support
Digital therapy through secure calls or chat removes stigma barriers and increases accessibility for individuals who avoid in-person consultations. It expands mental healthcare reach globally.
• Anonymous, private therapy access
• Psychological support anytime
• Higher adoption among youth & working class
4. Post-Surgery Follow-ups
Patients share progress and recovery updates virtually, reducing the need for multiple hospital trips after surgical procedures. Doctors can intervene faster when required.
• Track healing status remotely
• Immediate guidance & adjustments
• Less physical stress post-surgery
5. Remote Patient Monitoring (RPM)
IoT devices and wearables continuously push real-time vitals into the telemedicine system, enabling early detection and better clinical decision-making.
• Continuous vitals capture
• Automated alerts for anomalies
• Ideal for chronic & high-risk patients
6. Preventive Care & Wellness
Telemedicine apps also support lifestyle correction, preventive health planning, and habit tracking, reducing long-term healthcare burden.
• Diet, fitness & routine coaching
• Early detection through self-tracking
• Strengthens patient self-care behavior
Essential APIs for Building Telemedicine Apps
Using the right APIs can significantly lower development costs and accelerate telemedicine app deployment. Below are commonly used APIs and how they support different telehealth functionalities:
- Health Gorilla API → Enables access to EHR data, lab reports, and patient records while adhering to FHIR standards. Used for secure data exchange and risk management features.
- DrChrono API → Apple-affiliated API ideal for EHR-based telemedicine apps on iOS devices like iPhone and iPad. Popular for mobility-focused healthcare solutions.
- WebRTC API → Allows secure, real-time audio/video communication between patients and doctors with encrypted data sharing for virtual consultation.
- Validic API → Enables remote monitoring and simultaneous handling of 200+ patients’ health data. Supports personalized treatment plans and IoT wearable health tracking.
- Symptomate API → AI-driven symptom checker that lets users self-assess and identify probable conditions. Reduces dependency on initial consultations and speeds triage.
- TrueVault API → HIPAA-compliant storage solution for securely managing large-scale patient healthcare data inside telehealth platforms.
- HealthTap API → Offers the world’s largest verified doctor FAQ library, medical CRM capabilities, analytics tools, and AI-based triage matching patients with the right doctors.
What Are the Different Monetization Models of Telemedicine Applications?
There are various monetization models available to help telemedicine platforms earn consistently and scale revenue over time. Selecting the right mix is key to balancing user experience, operational efficiency, and business growth, even for digital wellness use cases like a Meditation & Mindfulness Assistant.
| Model | Description |
| Pay-Per-Visit | Patients pay per consultation, similar to traditional appointments. Simple to launch, and revenue depends on usage frequency. |
| Subscription Plans | Users pay monthly/yearly for unlimited or discounted care. Helps generate predictable recurring revenue and higher retention. |
| Freemium Model | Basic access remains free, while premium features and specialized services require paid upgrades. Great for fast user growth and upsell potential. |
| Commission-Based | The platform earns a percentage on every consultation completed by doctors. Revenue increases as more providers onboard and usage grows. |
| Insurance Partnerships | Insurance covers consultations directly inside the app. Boosts affordability and trust and drives high-volume adoption. |
| Product/Pharmacy Sales | Sell medicines, supplements, or devices inside the platform or via partners. Enables additional revenue linked to treatment decisions. |
How We Built a Telemedicine App?
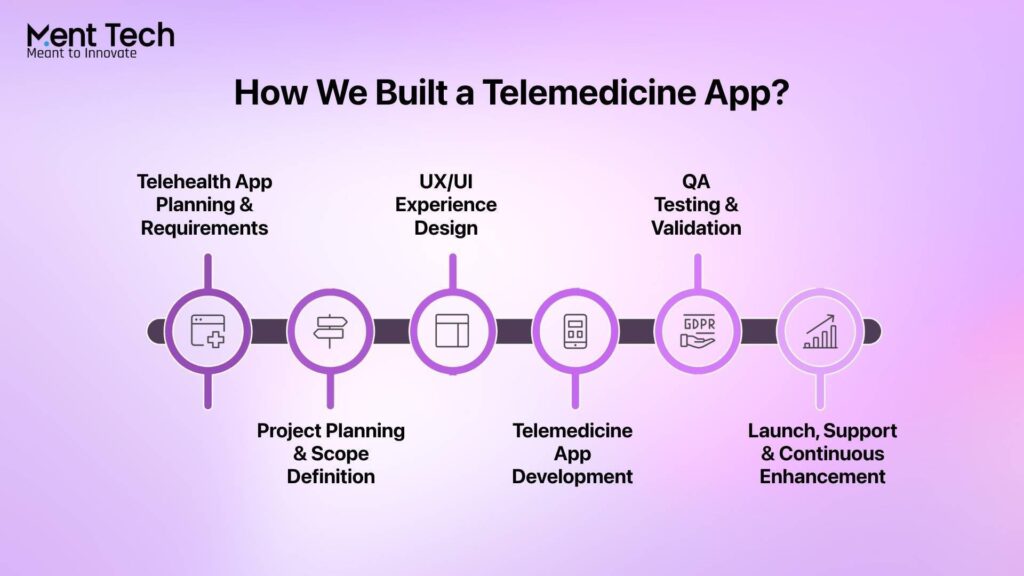
We build telemedicine apps through a structured process focused on usability, compliance, and scalability, resulting in a reliable platform that ensures smooth doctor-patient interaction and supports future AI Consulting driven enhancements.
1. Telehealth App Planning & Requirements
We start with deep market and compliance analysis and define core features, flows, and regulations to align with. This creates a clear foundation before development begins.
2. Project Planning & Scope Definition
Next, we finalize scope, timeline, budget, KPIs, and risk controls for structured execution. This ensures everyone is aligned and development moves with clarity and direction.
3. UX/UI Experience Design
Our designers craft simple, intuitive journeys for both patients and doctors. The goal is to make navigation effortless and interaction with virtual care extremely smooth.
4. Telemedicine App Development
We develop frontend, backend, and APIs, and core modules like chat, video calls, prescriptions, and payments. Agile sprint cycles help ship features faster while keeping scalability intact.
5. QA Testing & Validation
Every feature goes through rigorous functional, security, compliance, and performance testing. This ensures the platform is HIPAA-safe, reliable, and ready for patient use.
6. Launch, Support & Continuous Enhancement
We launch as an MVP or full version and then monitor usage, optimize performance, and enhance features. Regular updates and audits keep the app secure, stable, and future-proof.
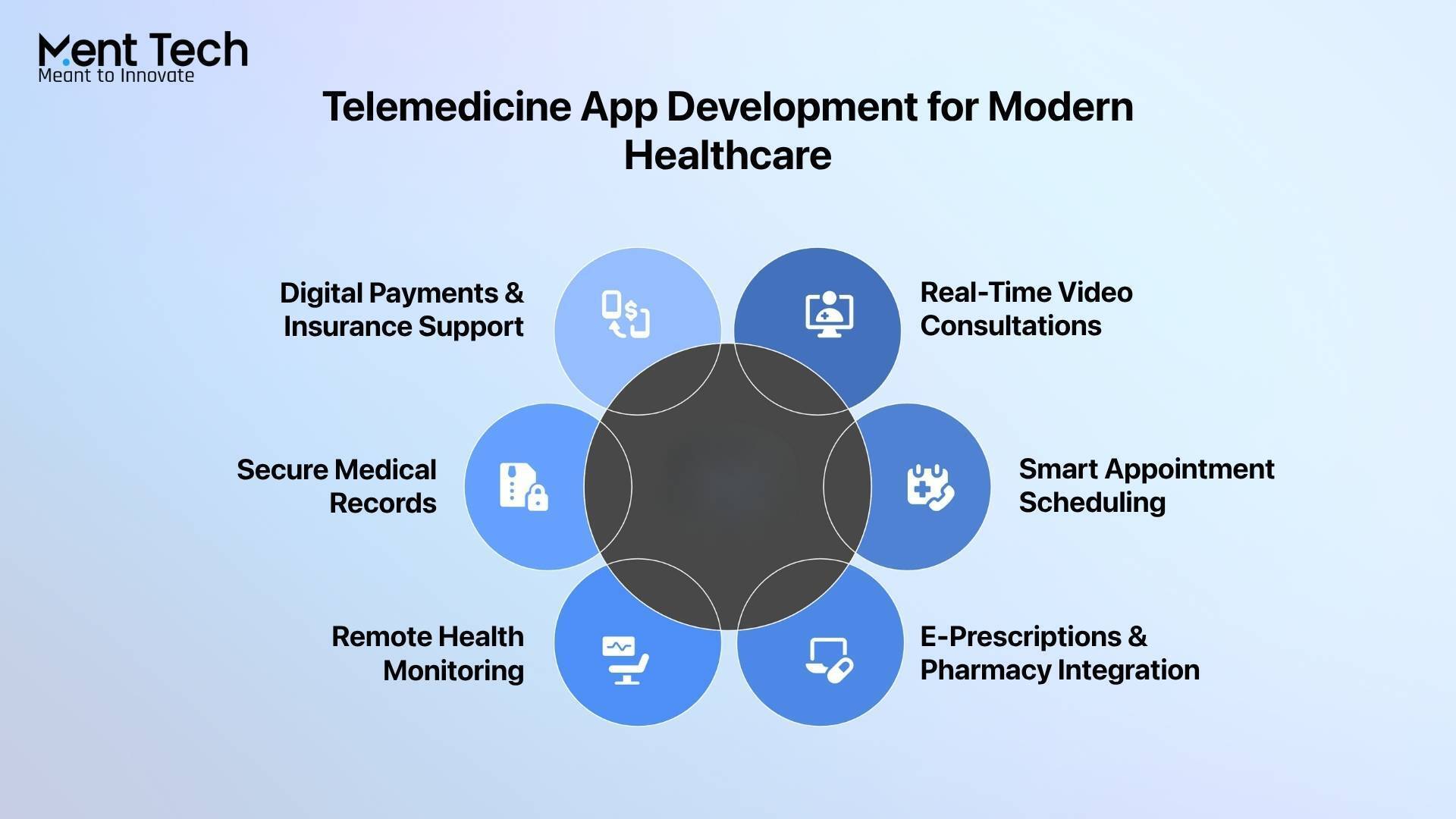
Must-Have Features in a Modern Telehealth Platform
A modern telemedicine solution must offer secure, smooth, and fully connected digital healthcare, going beyond simple video calls to deliver end-to-end virtual care experiences.
1. Secure User Authentication
Patients and doctors should log in safely with multi-factor authentication. HIPAA and GDPR compliance are essential for data protection.
2. Video Consultations & Real-Time Chat
High-quality video calls and instant chat enable smooth remote care. Support for file sharing (reports, scans) enhances diagnosis accuracy.
3. Appointment Scheduling & Reminders
Easy booking, rescheduling, and cancellation improve user convenience. Automated reminders reduce missed appointments.
4. E-Prescriptions & Pharmacy Integration
Doctors can issue digital prescriptions instantly, while pharmacy links allow patients to order medicines directly through the app.
5. Payment Gateways & Insurance Support
Secure digital payments and insurance processing make the platform easier to use end-to-end for both patients and providers.
Future Trends in Telemedicine App Development You Should Know
Telemedicine is advancing quickly, and the future will be driven by smarter automation, real-time health data, and intelligent diagnostics. AI will streamline triage, accelerate symptom evaluation, and improve clinical decision-making, while IoT and wearables will push continuous patient vitals into telehealth systems, enabling proactive care and faster interventions without physical visits, opening new growth opportunities similar to how AI as a Service models scale digital healthcare delivery.
Parallel to this, the next decade of telehealth will be shaped by privacy-first architecture and immersive virtual care experiences. Blockchain will secure medical data through tamper-proof record exchange, and AR/VR will enable guided remote procedures and advanced training. Combined with 5G’s ultra-low latency video performance, telemedicine will shift from a support channel to a primary mode of care delivery worldwide.
Conclusion
Telemedicine apps are redefining modern healthcare by making consultations faster, care delivery more accessible, and remote patient monitoring more achievable. This shift isn’t just about convenience. It’s about enabling providers to deliver better outcomes, improved continuity of care, and more scalable treatment models for today’s digital-first patients.
Ment Tech, a leading healthcare development company, builds secure, compliant, and high-performing telemedicine platforms. From remote monitoring and chronic care to virtual triage and specialist integration, we deliver efficient, customized digital healthcare solutions designed for modern patient needs. Contact us today to discuss how we can help make your telemedicine product vision a reality.
FAQs-
Telemedicine platforms can monetize through pay-per-consultation, subscription plans, provider onboarding fees, insurance reimbursements, white-label licensing, marketplace referral commissions, and remote patient monitoring service fees, especially when supported with scalable AI Development models aligned for healthcare.
Yes, but only if regulatory, licensure, data privacy, and medical practice compliance requirements of each region are followed. Global rollout requires regional provider licensing, data localization policies, and secure cross-border interoperability.
Apps must follow HIPAA, HITECH, DEA prescribing rules, FDA oversight for regulated diagnostics/medical devices, and secure ePHI handling standards. Privacy-first architecture, protected data flow, audit trails, and encrypted communications are mandatory.
A modern telehealth platform uses end-to-end encryption, role-based access, multi-factor authentication, secure API gateways, protected cloud storage, and zero-trust security frameworks. Regular audits + continuous security monitoring ensure safe PHI management.
Yes. Telehealth can connect with EHRs like Epic, Cerner, and athenahealth, using FHIR, HL7, and HIPAA-compliant API integrations to sync patient records, clinical workflows, lab data, billing, and scheduling without friction.
Cost varies based on feature complexity, level of regulatory compliance, number of integrated systems (EHR, wearables, pharmacy), custom UX, security measures, tech stack, scalability needs, and post-launch support, especially when advanced Multimodal AI capabilities are involved.